January is Cervical Cancer Awareness Month and serves as a reminder to all women to speak with their physicians about the risks of developing cervical cancer, what causes it, and how it can do to prevent it. Thankfully cervical cancer is a highly preventable and treatable cancer, thanks to improved screening and vaccination.
It’s a common misconception that smear tests are carried out to check for cervical cancer; they are actually designed to pick up any precancerous changes – which means any variations or abnormalities in the cells that have the potential to become cancerous. Getting regular check-ups means that any abnormalities are picked up early and therefore much more treatable than if they were left for a long time.
Because cell changes can occur many years before cancer develops, the cervical screening programme has been very successful, overall.
Because smears are a private and intimate examination, some women are put off by the idea, But the procedure is nothing to be feared.
In a bid to demystify the pap smear test a bit, here’s an idea of what to expect when you go for the test.
During a smear test, the clinician needs to examine the surface of your cervix, which is the neck of the womb, and take a swab of cells from the area. The procedure is similar to the one used to test for sexually transmitted infections, however a soft brush or spatula is used instead of a cotton bud.
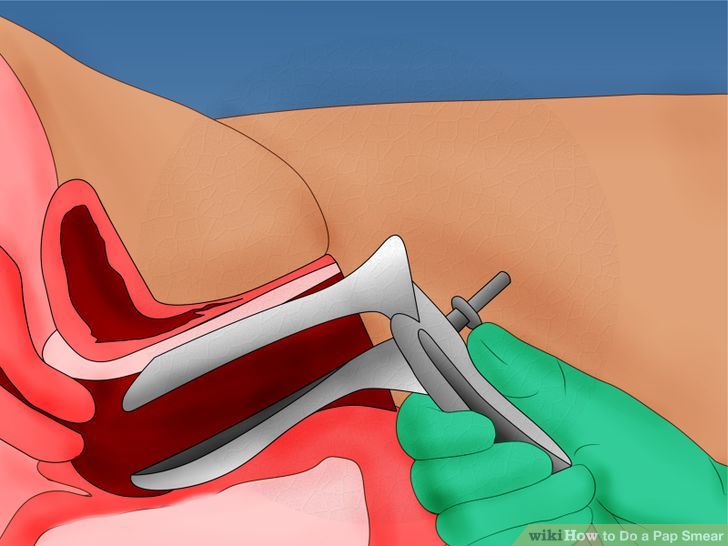
You will be asked to undress from the waist down and lie on a couch, with your legs bent and open. The clinician then inserts a plastic (or metal) tong-like instrument called a speculum into your vagina. The speculum is usually about 8cm long – but it comes in different sizes, depending on the woman.
When the speculum is inside, the clinician squeezes the handles, opening the walls of the back of the vagina, to about 5-8cm wide. They are then able to see the cervix in all its glory and look for any irregularities on the surface, sometimes using a light to help. Then a soft brush is inserted and gently twirled around to collect a swab of cells from the area. The procedure is over in about five minutes.
The procedure can be a little uncomfortable, but it shouldn’t be painful. Sometimes it can be difficult to visualise the cervix, so might take a bit longer. If you are in any pain or discomfort, tell the clinician. And try to relax, as tension makes the procedure harder to carry out.
Occasionally, women might experience a bit of spotting afterwards. This is not unusual and shouldn’t be a cause of worry.
What happens next?
The clinician will send your cells off to the lab for testing and you should get your results after two weeks. Most test results show that everything is normal. Only in one in 20 cases will there be abnormalities.
If you have an abnormal smear it’s important not to panic. most abnormal cells will not be cancerous, and will often change back on their own. In some cases, they will need to be removed.
Statistically, there is a very small risk that a woman with an abnormal smear will develop cervical cancer – about one in 2,000.
If minor changes to cells are found, or the sample taken was not sufficient, then you will be invited back for a second smear. If more significant changes are detected, you’ll be referred to a specialist clinic for a procedure called a colposcopy. This procedure is similar to a smear: a microscope is inserted into your vagina to allow for a closer examination of the cervix. The colposcopist may take a tissue sample and will be able to determine whether further treatment is needed.
Now that you know what to expect, hopefully you’re not fearful of the procedure anymore and understand it’s importance and will add it to your list of resolutions for the new year.






