Heavy menstrual bleeding (HMB) is also known as menorrhagia. This medical term refers to abnormally heavy or prolonged bleeding.
For some women with HMB, It can be challenging to carry out regular daily living activities with HMB because of significant blood loss. And some bleeding can be very heavy, leading to the need to change your pad more often (less than two hours). If this sounds like you and your periods, talk with your health care provider about possible treatment options.
Various things can cause heavy menstrual bleeding. Some of these causes include:
- Fibroids and polyps: Uterine fibroids and uterine polyps may cause increased bleeding and irregular periods.
- Adenomyosis: This causes endometrial tissue (lining of the uterus) to grow inside the uterine wall. It’s seen in later childbearing years and usually resolves following menopause.
- Endometriosis: This condition causes endometrial tissue to grow outside of the uterus. This growth can occur on the ovaries and supporting ligaments of the uterus and in the pelvic cavity.
- Irregular ovulation: When ovulation and periods don’t occur regularly, areas of the endometrium (the uterine lining) can become too thick. This irregularity usually happens during puberty, perimenopause, and in people diagnosed with polycystic ovary syndrome and hypothyroidism.
- Bleeding disorders: Some medical conditions prevent blood from clotting properly, which leads to heavy bleeding.
- Medications: Blood thinners can cause heavy menstrual bleeding.
- Intrauterine devices (IUD): IUDs, particularly those containing copper, may also cause heavier menstrual bleeding, especially during the first year following insertion.
- Cancer: Heavy menstrual bleeding can be an early sign of uterine or cervical cancer. Most cases happen in people in their mid-60s who are postmenopausal. With early diagnosis, treatment is highly effective.
- Other causes: Heavy bleeding can be pregnancy-related, in the event of ectopic pregnancy or miscarriage. Pelvic inflammatory disease also can cause heavy menstrual bleeding. Other times, the cause is unknown.
When should you see a doctor
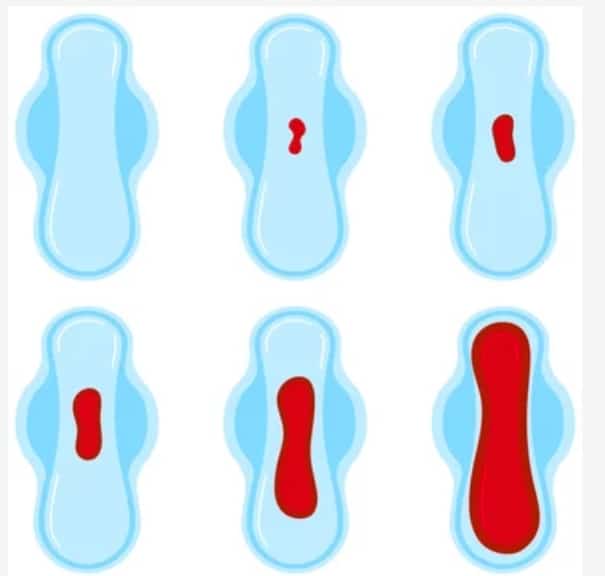
It can be tricky to determine if your menstrual bleeding is considered heavy or not, because every woman has a different idea of what heavy bleeding actually is.
Typically, menstrual bleeding lasts about four to five days, and overall blood loss is minimal (two to three tablespoons). It’s worth noting that menstruation isn’t just blood. It also contains endometrial tissue, so it’s not always easy to estimate actual blood loss.
According to the American College of Obstetrics and Gynecology (ACOG), any of the following are signs of heavy menstrual bleeding:
- Bleeding that occurs for more than seven days
- Needing to use a tampon and a pad simultaneously or using more than one pad to prevent leaking
- Vaginal bleeding that’s heavy enough to soak at least one pad each hour for more than two hours straight
- Needing to get up in the middle of the night to change pads
- A menstrual flow that includes blood clots that are the size of a large coin or larger
- Irregular vaginal bleeding or bleeding between periods (that isn’t ovulation spotting)
Heavy bleeding can cause anemia, which will make you feel constantly tired.
If you’re experiencing heavy periods and notice the signs mentioned above, it’s important to speak to your health care provider. They may want to see you to evaluate your symptoms further.
How can you tell if the blood loss is severe
You might be asking, when should you go to the hospital for heavy menstrual bleeding? Blood loss from heavy periods can lead to a more severe, urgent medical condition. Heavy blood loss can decrease the amount of circulating blood in the body and the amount of oxygen usually needed by the body. So, can losing too much blood during your period be life-threatening? The answer is, if you’re experiencing any of the following while you have heavy vaginal bleeding, you should seek immediate medical attention:
- Shortness of breath
- Chest pain
- Increased heart rate
- Dizziness
- Faintness
Treatment of HMB
Treatment options for HMB vary based on the cause, patient age, general health, medical history, medications currently being taken, and the extent of bleeding during each menstrual cycle. Your health care provider may also carry out further investigations like blood work or ultrasound to determine the best method of treatment for you.Fertility plans may also be a factor in the type of treatment prescribed.
Ultimately, most people want to reduce the bleeding associated with HMB. Fortunately, there is help for this. Speak up and find the help you need.