For a country where abortion is illegal and all forms of premarital sex generally frowned upon, quite a large number of women are familiar with the term “D and C” even though many also do not know what the letters stand for.
A D&C is a Dilation and Curettage which is a surgical procedure where the cervix is dilated (expanded) so that the lining of the womb can be scraped with a curette to remove “abnormal” tissues. This procedure may be done for several reasons, including to diagnose certain conditions however the most common reason why this procedure is done is to remove unwanted pregnancy.
When this procedure is not properly done, i.e if the person doing it gets a little overzealous with the curette it can cause damage and formation of scar tissue in the uterine cavity with may eventually lead to a condition called Asherman’s syndrome.
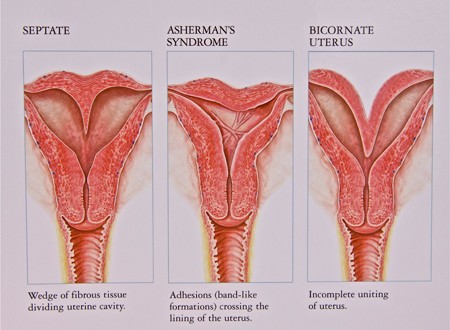
Asherman syndrome is the formation of scar tissue in the uterine cavity. In most cases, it occurs in women who have had several dilatation and curettage (D&C) procedures or any other instrumentation of the uterus. Including curettage for post-partum complications such as post-partum hemorrhage or retained placenta or other uterine surgery such as removal of fibroids.
A severe pelvic infection unrelated to surgery may also lead to Asherman syndrome.
Intrauterine adhesions can also form after infection with tuberculosis or schistosomiasis although this is not common at all.
Symptoms caused by Asherman’s syndrome
Asherman’s syndrome can be with or without symptoms. Symptoms that women may present with include:
- Infertility
- Recurrent pregnancy loss (miscarriage)
- Menstrual irregularities such as very light periods (hypomenorrhea) or absence of periods (amenorrhea). This can occur if scar tissue replaces the normal endometrium, so there is less endometrium shed during menses. It also can occur if scar tissue blocks the outflow of the menstrual blood.
- Cyclic pelvic pain can occur if scar tissue blocks the outflow of the menstrual blood, causing uterine cramping and pelvic discomfort or pain.
However, all these symptoms could be related to several conditions. They are more likely to indicate Asherman syndrome if they occur suddenly after a D&C or other uterine surgery.
Diagnosing Asherman’s syndrome
The sure fire way to diagnose Asherman’s syndrome is to directly look at the uterine cavity and scar tissue using hysteroscopy however this is not commonly available here in Nigeria so alternatively a Hysterosalpingogram (HSG) may be done. This involves injection of dye into the uterine cavity followed by an X-ray – or a sonohysterogram -injection on fluid into the uterine cavity while looking with an ultrasound.
Transvaginal ultrasound can be used to evaluate and measure the endometrial stripe (thickness of the endometrial lining).
An endometrial biopsy is sometimes performed to sample the lining to the uterus as a way of determining if any normal endometrium is present.
Classification/staging.
There are three stages of disease: Stage I (mild), Stage II (moderate) and Stage III (severe). The stage of disease is determined by the extent of the endometrial cavity involved (adhesions throughout the uterus or just in a small area), the type of adhesions (filmy or dense) and the menstrual pattern.
For example, mild disease can involve just a few bands of scar tissue in a woman with normal periods. Severe disease can be characterized by complete obliteration and occlusion (obstruction) of the endometrial cavity and no menstrual bleeding.
Treatment
In general, the treatment involves breaking up the scar tissue and preventing re-growth of scar tissue. If a woman has intrauterine adhesions, but does not have any symptoms (such as cyclic pelvic pain) and is not concerned about having children, there is no medical reason why intrauterine scar tissue needs to be treated.
The treatment of Asherman’s syndrome involves two stages:
1. Hysteroscopic lysis of adhesions (removal of scar tissue)
The first step in the treatment of intrauterine adhesions is to break up the scar tissue, open the uterine cavity and identify the tubal ostia (openings of the fallopian tubes into the uterus). Ideally this is done using a hysteroscope to break up the scar tissue under direct visualization.
The surgery can be performed in the office or in the operating room, depending on the patient and the extent of her adhesions. This is usually a day case, with a rapid recovery and minimal need for post-operative pain medication.
If the scar tissue is thin and filmy, it can be broken up bluntly using the hysteroscope. If the adhesions are thick and dense, scissors are used to cut the scar tissue. Ultrasound is sometimes used to help guide the lysis of adhesions.
2. Preventing reformation of the scar tissue after the initial lysis of adhesions
One of the challenges with Asherman’s syndrome is that once the scar tissue is removed, it sometimes comes back. Techniques to prevent the reformation of scar tissue include the use of estrogen post-procedure, repeat office hysteroscopies to break up scar tissue as it forms, and placement of a balloon in the uterine cavity after lysis of adhesions:
3. Oral Estrogen: Women are sometimes given a course of estrogen (typically for 30 days) after they undergo a hysteroscopic lysis of adhesions as a way of promoting growth of normal uterine lining and helping prevent the regrowth of the scar tissue.
4. Repeat office hysteroscopy: Sometimes a repeat office hysteroscopy seven to 14 days after the initial hysteroscopic lysis of adhesions is recommended. During this procedure, a small flexible hysteroscope is used to identify any scar tissue that may have reformed and the hysteroscope is used to bluntly break up this scar tissue. This cycle is repeated every seven to 14 days until no re-growth of scar tissue is seen, but typically not more than three times total.
5. Placement of an intrauterine balloon: Some practitioners place an inflated balloon or an intrauterine device (IUD) inside the uterine cavity after the initial lysis of adhesions to try to prevent re-growth of scar tissue.
Unfortunately, as i stated earlier hysteroscopy is not widely available in Nigeria therefore many hospitals offer a “blind” adhesiolysis which also provides symptomatic relief to the patient even though it is not the gold standard.
The more important thing is to try and prevent Asherman’s completely by seeing a qualified specialist if there is any need for intrauterine instrumentation or if any of the above symptoms is noted after any gynecological procedure.






